Manalapan
(732) 845-0100
Manalapan (732) 845-0100
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.

Surgery for flat feet, or pes planus, aims to correct the underlying structural issues in the foot and alleviate associated symptoms. The surgical approach depends on the severity of the condition and the individual's symptoms. In cases where conservative treatments such as wearing orthotic inserts fail to provide relief, surgical intervention may be considered. One common surgical procedure for flat feet is the realignment of the bones and tendons in the foot to restore the arch and improve stability. This may involve techniques such as tendon transfers, osteotomies, which are bone cuts, or fusion procedures to correct deformities and improve foot function. Another option is the insertion of implants or grafts to support the arch and provide long-term stability. Surgical correction of flat feet requires careful evaluation and planning by a qualified podiatrist to ensure optimal outcomes and minimize risks. If you have flat feet that are causing you pain, it is suggested that you consult with a podiatrist who can determine if surgery is an option for you to consider.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Dr. Charles Marchese of Manalapan Foot & Ankle. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
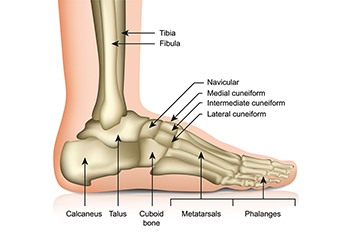
Though cuboid syndrome predominately affects athletes, non-athletes can suffer from it too. Cuboid syndrome is also called cuboid subluxation or cuboid fault syndrome, and occurs when a joint or ligament near the cuboid bone of the foot becomes damaged, or when the bone itself is dislodged from its natural position. Pain may be persistent, or come and go, and it is usually marked by the outside of the foot. Cuboid syndrome, unless severe, can be difficult to diagnose. A doctor will likely ask questions about how long the pain has been present, and will apply pressure on the cuboid bone to determine the origin of pain.
There are a number of causes that can lead to the syndrome. Due to athletic activities, repeated stress placed on the foot can cause cuboid subluxation. Ballet dancers, runners, and other athletes often develop this condition. Basketball or tennis players may also develop this condition, as they place stress on their feet while moving side to side. Cuboid syndrome can often develop over time; however it can come out of a sudden injury as well. Over pronation, or other problems with feet, can exacerbate the condition if not corrected.
Among podiatrists, there is some disagreement about the treatment, as well as the definition of cuboid syndrome. Some see the injury as an injury to the ligaments located nearby the cuboid bone, while others believe it refers to the dislocation of the calcaneal-cuboid joint only. Treatment opinions differ as well. Although it can be treated by manipulation in order to reposition the bone, this must be done with extreme care in order to avoid injury. Some doctors, however, prefer treatment through the use of orthotic pads, designed to keep the bone in its place. Effectiveness of these treatments may vary, according to the severity of the injury.
When you experience side foot pain, it is important that you seek medical assistance. If a subluxed cuboid is caught and treated early, treatment is usually successful, and individuals may begin activities such as sports when the pain subsides. If left untreated, the pain will worsen, and the condition could cause permanent damage.
Athletes often develop various foot issues. A male ballet dancer experiences sudden lateral foot pain after landing from a jump, fearing it may end his career. A basketball player suffers acute pain after twisting his ankle during a game, and is now using crutches. A female ballet dancer faces persistent lateral foot pain hindering her rehearsals, despite treatments over two years. These cases share a common condition often overlooked and known as cuboid subluxation. This involves injury to the joints and ligaments around the cuboid bone, causing lateral foot pain and weakness during push-off. Diagnosis involves physical examination, as imaging may not clearly show the condition. Treatment includes manipulation to realign the cuboid, followed by supportive measures like taping and orthotics. Addressing biomechanical issues is important for recovery, ensuring athletes can return to their activities safely. If you are an athlete and have foot pain, it is suggested that you schedule an appointment with a podiatrist as soon as possible to prevent worsening of symptoms and obtain appropriate treatment for the diagnosis.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with Dr. Charles Marchese from Manalapan Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
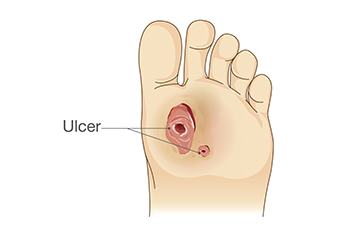
A diabetic foot wound refers to an open sore or ulcer that develops on the foot of individuals with diabetes, typically due to a combination of factors including neuropathy, poor circulation, and impaired wound healing. Neuropathy, a common complication of diabetes, causes nerve damage that diminishes sensation in the feet, making individuals less aware of injuries or pressure points that can lead to wounds. Poor circulation, another consequence of diabetes, reduces blood flow to the feet, hindering the delivery of oxygen and nutrients necessary for wound healing. These factors, coupled with compromised immune function, increase the risk of infections and slow the healing process. Symptoms of diabetic foot wounds may include redness, swelling, warmth, drainage, and foul odor. Recognizing these signs is crucial for prompt intervention and prevention of complications such as infections and amputations. If you have diabetes and have developed a foot wound, it is strongly suggested that you are under the care of a podiatrist who can provide you with the proper wound care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Charles Marchese from Manalapan Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.

Hallux limitus is a condition where the big toe joint gets sore, stiff, and inflamed. If not treated, it can turn into hallux rigidus, where the joint cannot move, causing a lot of pain and difficulty walking. To help with these issues, foot doctors focus on making the joint move better to reduce pain and improve how it works. They often use special shoe inserts with a deeper heel and a part that supports the inside of the foot. The doctors also look at whether the problem is because the joint does not work well or if it is because of the shape of the foot. Depending on the issue, they may use different kinds of inserts. They usually avoid certain materials and features that can make things worse. When making these inserts for everyday shoes, podiatrists think about things like foot strength and how the foot lines up. They may suggest exercises, massage, and good shoes. If you have a stiff and painful big toe, it is suggested that you schedule an appointment with a podiatrist for treatment, which may include orthotics.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Charles Marchese from Manalapan Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.