Manalapan
(732) 845-0100
Manalapan (732) 845-0100
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.

Anyone who is active physically on a regular basis is a prime candidate for stress fractures. Among the main causes of these hairline cracks in a bone are changing your workout program, improper footwear, and improper technique. Going from running on turf to running on a road or other hard surface also may put you at risk. High-impact sports, such as soccer, running, basketball and dance, increase the likelihood of sustaining stress fractures. Non-athletes can also develop stress fractures, usually by increasing activity after refraining for a long time. Having osteoporosis and vitamin D deficiency, especially common among postmenopausal women, is another risk factor. If you have sustained stress fractures in the past, you are more likely to experience them again. If you suspect you may have developed stress fractures in your feet, it is a good idea to consult a podiatrist who can conduct a thorough examination and offer appropriate treatment options to reduce your pain.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Dr. Charles Marchese from Manalapan Foot & Ankle. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.

Heel fissures are another name for the medical condition known as cracked heels. This ailment can cause discomfort and the heels may bleed in severe cases. Cracked heels can develop for a variety of reasons such as wearing shoes that are backless, or from standing on hard surfaces for the majority of the day. Additionally, the aging process may contribute to the onset of cracked heels which could lead to less padding in the heel area. It is often an unsightly condition and the skin may harden or turn a yellowish color. Patients who are diabetic may need to take extra precautions when looking for any cracks in the skin as they can become infected. Diabetic patients can often have difficulty feeling anything on their feet as a result of elevated blood sugar levels. There may also be existing medical conditions that can lead to cracked heels including eczema, thyroid disorders, and rheumatoid arthritis. If you have developed cracked heels, please schedule an appointment with a podiatrist who is able to prescribe the correct treatment that can bring relief.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Dr. Charles Marchese from Manalapan Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
Ways to Prevent Cracked Heels
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
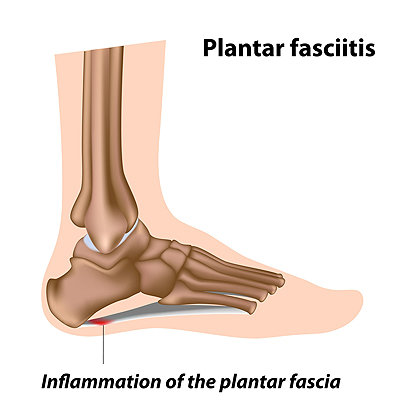
Elderly people often develop foot problems and one of the most common is plantar fasciitis. Plantar fasciitis occurs when the plantar fascia ligament that connects the heel to the front of the foot is damaged by tiny tears. It is caused by repetitive injury or excessive strain which causes pain in the heel area of the foot and is most unbearable when first rising or after prolonged sitting. As with any disorder, this ailment can be prevented to some degree. There are a variety of things seniors can do to help ward off painful food disorders. Getting a gait analysis so that if there are issues with posture or the way one walks, they can be detected and corrected. Regularly stretching the calves and ankles can help prevent tight muscles and tendons that cause small tears in the heels of the feet. Wearing well-fitting, supportive shoes, with proper cushioning and arch support can reduce pressure on feet and help make walking and performing other activities more comfortable. Placing inserts that have deep heel cups and elongated cradles for the arches into regularly worn shoes can be used to assist with a flatter foot as one ages. If you are a senior or taking care of a senior who suffers from painful foot conditions like plantar fasciitis, it is suggested you see a podiatrist to have the feet evaluated and effective treatment prescribed.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Charles Marchese from Manalapan Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.

Most blisters form due to the constant rubbing of the skin with the inside of your shoe. This forms tears in the layers of skin which signals your body to protect it from further distress. In this case, fluid forms a cushion of sorts between the torn skin (epidermis) and the uppermost layers underneath the epidermis. The usual cause is ill-fitting shoes worn over long periods of time. In addition, a narrow toe box, too much room in the heel, and raised seams inside the shoe can also cause blistering. Besides forming on the side of the toes, blisters can form on the bottom of the toes too. Seams in socks can cause blisters on the top of your toes, and protruding bunions and hammertoes are frequent sites for blisters to form. Blisters may be worse if the feet get wet, so wearing socks that wick moisture from the skin may help to reduce them. If you have recurring or infected blisters, it is a good idea to see a podiatrist who can treat them safely as well as provide various prevention methods.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Dr. Charles Marchese of Manalapan Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our offices located in Manalapan, NJ, and Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.